by: Ramachandran Srinivasan, MD., FACR

Gout is a painful and debilitating condition that develops in some people who have chronically high blood levels of urate (commonly referred to as uric acid) that leads to tophus (lump nodules formation), arthritis, hypertension, heart and renal failure.
RISK FACTORS — Gout is most common in men between 30 and 45, and in women between ages 55 and 70. It is estimated that gout affects approximately 2 percent of people in the United States. The following characteristics increase the risk of developing gout:
· Obesity
· High blood pressure
· Consuming excessive amounts of alcohol (particularly beer, whiskey, gin, vodka, and rum) on a regular basis
· Taking medications that affect blood levels of urate (especially diuretics)
· Ingesting large amounts of meat and seafood
· Overeating
· Fasting
· Injury or recent surgery
· Elevated uric acid levels in cancer, kidney diseases, and other
SYMPTOMS — Gout attacks cause sudden severe joint pain, sometimes with redness, swelling, and tenderness of the joint. Although an attack typically affects a single joint, some people develop a few inflamed joints at the same time. The pain and inflammation are worst within several hours, and generally improve completely over a few days to several weeks, even if untreated.
The characteristic pain and inflammation of gout develops when a type of white blood cell, called neutrophils, attempt to surround and digest urate crystal deposits. White blood cells are the body’s first line of immune defense and recognize the crystal deposits as foreign material. Chemical signals released by other types of white blood cells and cells in the joint contribute to the pain, swelling, and redness associated with a gout attack.
PHASES OF GOUT — There are three main phases of gout: acute gouty arthritis, intercritical gout, and chronic tophaceous gout.
Acute gouty arthritis — Attacks of gout usually involve a single joint, most often the big toe or knee. This attack is known as acute gouty arthritis. People with osteoarthritis in the fingers may experience their first gout attacks in the fingers rather than the toes or knees.
Intercritical period — The time between gout attacks is known as the intercritical period. A second attack typically occurs within two years, and additional attacks may occur thereafter. If gout is untreated over a period of several years, the time between attacks may shorten and attacks may become increasingly severe and prolonged. Over time, the attacks can begin to involve multiple joints at once and may be accompanied by fever.
Chronic tophaceous gout — People who have repeated attacks of gout over many years can develop tophaceous gout. This causes large numbers of urate crystals to collect in joints, bones, and cartilage. The urate collection causes a nodule or mass called a tophus (plural tophi) to form. The tophus causes resorption and erosion of the bone, and can potentially cause deformity

The presence of tophi near the knuckles or small joints of the fingers can be a distressing cosmetic problem. Tophi are usually not painful or tender. However, they can become inflamed and cause symptoms like those of an acute gouty attack.

Tophaceous gout was more common in the past, when treatment for hyperuricemia was unavailable. Certain groups are still at risk for tophaceous gout, including:
- People who are treated with cyclosporine after organ transplantation
- Those who cannot tolerate adequate doses of medications to treat hyperuricemia (for example, due to kidney failure or drug allergy)
- Women who are postmenopausal, especially those taking a diuretic
The risk factors listed previously can also contribute to the development of tophaceous gout.
URINARY COMPLICATIONS — People with gout are at increased risk of developing kidney stones. Uric acid crystals can collect in the urinary tract and form a stone. If a stone is large enough, it can block one of the tubes (ureters) that carry urine from the kidney to the bladder and out of the body.
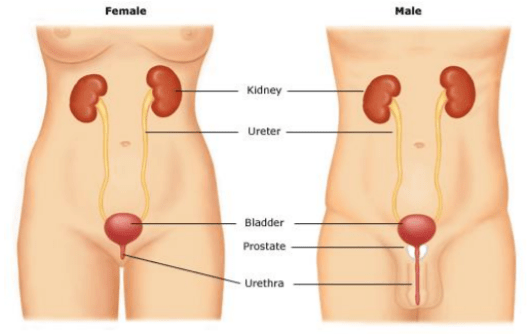
Rarely, urate crystals collect in the kidney tissue itself, where they can cause inflammation and scar tissue, which reduce kidney function. Medications that increase the amount of uric acid excreted by the kidneys may help to reduce the risk of developing kidney stones. Hyperuricemia or excess uric acid can lead to kidney failure, hypertension, and cardiovascular problems.
DIAGNOSIS — There are many illnesses that can cause joint pain and inflammation. Gout is strongly suspected if a person has an acute attack of joint pain, followed by a period when there are no symptoms. It is important to confirm the diagnosis of gout to ensure that potentially harmful medications are not taken unnecessarily over a prolonged period of time.
The best way to diagnose gout is to examine synovial fluid from an affected joint, to look for urate crystals in the sample. To obtain the fluid, the provider uses a needle and syringe to withdraw a small amount of fluid from inside the joint. Tophi located just beneath the skin can be sampled with a needle to diagnose tophaceous gout.
However, some people do not have urate crystals in their synovial fluid when symptoms are present. In this case, the diagnosis is based upon a person’s symptoms and a physical examination. Criteria for diagnosing gout include:
- A history of pain and inflammation involving one joint at a time, especially the joint at the base of the large toe
- Complete resolution of symptoms between attacks
- Blood testing showing high levels of urate
- Rapid improvement in joint inflammation after treatment with colchicine
TREATMENT OF GOUT ATTACKS — The goal of treatment of flares of gouty arthritis is to reduce pain and inflammation quickly and safely. It may be necessary to use more than one drug to achieve this goal. Deciding which medication to use is based upon several factors, including a person’s risk of bleeding, their kidney health, and whether there is a past history of an ulcer in the stomach. Anti-inflammatory medications are the best treatment for acute gout attacks and are best started early in the course of an attack.
People with a history of gout should keep medication on hand at all times to treat an attack because early treatment is an important factor in decreasing the pain and severity of an attack. Nonsteroidal anti-inflammatory drugs — Nonsteroidal anti-inflammatory drugs (NSAIDs), work to reduce swelling in a joint, and include ibuprofen (Advil®, Motrin®) and indomethacin (Indocin®)
NSAIDs are generally recommended for people who have no history of kidney or liver disease, no bleeding problems, do not use anticoagulant medications (blood thinners such as warfarin or Coumadin®), and who have no history of a stomach or duodenal ulcer.
NSAIDs are most effective in the treatment of a gout attack when they are started as soon as possible, before the attack is full blown. People who have had previous attacks may start taking an NSAID at the first signs of a recurrence.
Although aspirin is an NSAID, it is not usually recommended for the treatment of gout because of it’s potential impact on levels of urate in the blood.
Colchicine — Colchicine may be prescribed instead of an NSAID. Colchicine does not increase the risk of ulcers, has no known interaction with anticoagulants, and in proper doses, does not affect kidney function. However, colchicine can have bothersome side effects, including diarrhea, nausea, vomiting, and crampy abdominal pain. For this reason, colchicine is generally reserved for patients who cannot tolerate NSAIDs. Some people have a great deal of success with colchicine and do not have side effects; colchicine might be used first for this group. Colchicine is generally taken as a pill.
Steroids — Steroids, also known as glucocorticoids, are effective anti-inflammatory agents. Commonly used oral steroids include prednisone, prednisolone, and methylprednisolone. Steroids may be used if NSAIDs and colchicine cannot be used. They may be injected directly into the affected joint (called an intraarticular injection) or they can be given as pills or by intramuscular injection. People who have multiple affected joints or who cannot take NSAIDs or colchicine may be given oral steroids. However, there is an increased risk of recurrent gout attack (called rebound) in people who take oral steroids. For this reason, steroids should be tapered slowly over a period of seven to 10 days.
PROPHYLACTIC THERAPY — Prophylactic therapy aims to prevent or reduce the occurrence of acute flares of gouty arthritis. Colchicine is usually recommended as prophylactic therapy; it is taken daily at low doses to avoid gastrointestinal side effects. Colchicine reduces the frequency of acute gout attacks, particularly while starting other drugs that lower urate levels. Prophylactic colchicine is not usually used as a long-term (years) treatment, but is a helpful bridge as a person progresses from an acute flare to preventive therapy. Although not as well documented as colchicine, daily NSAIDs are sometimes used for prophylactic therapy, and may have an advantage (because of pain relieving properties) for people who also have osteoarthritis.
PREVENTIVE THERAPY — Preventive therapy includes medications and dietary changes that can be used long-term to lower urate levels and prevents the progression of gout. Progressive gout can cause bone destruction and deformity (gouty arthropathy), disability, kidney stone formation, and, possibly, kidney damage. People who have one or more of these complications are strongly encouraged to take a urate lowering treatment.
Not everyone with gout will require preventive therapy; those who have rare or mild attacks are often able to manage their gout by treating the acute attacks alone. On the other hand, people with sporadic gout flares that are unusually prolonged, painful, and/or disabling are often encouraged to take preventive therapy.
Medications — Urate-lowering or antihyperuricemic medications lower urate levels by helping to eliminate or decrease production of uric acid. Antihyperuricemic therapy is usually started after a gout attack has resolved. People who take their medication regularly experience fewer attacks. At present, preventive therapy is recommended indefinitely because there is no benefit to taking a break from medication.
Probenecid increases the efficiency of uric acid excretion by the kidney, and is called a uricosuric drug. Benzbromarone is a more potent uricosuric drug, but is not available in the United States. Both drugs can cause side effects, including rash, stomach upset, and kidney stone formation.
Losartan is used to treat high blood pressure but also has a useful, though weak, urate-lowering effect, as does the lipid-lowering drug fenofibrate.
Allopurinol works by preventing the formation of uric acid. It is the most commonly used drug for lowering urate levels in gout. Allopurinol can cause side effects, including rash, lowered white cell and platelet counts, diarrhea and fever, although these problems occur in a relatively small percentage of patients.
Lowering urate levels is a process that can take weeks or months. Very rapid urate lowering can cause acute flares of gout. Medications to lower urate are generally started at a low dose and increased slowly until the blood urate level is reduced and maintained at a level where urate crystal formation is unlikely. Increased fluids are recommended during this time (at least two liters per day are recommended).
The prophylactic therapy (colchicine or NSAIDs, may be discontinued when blood levels of urate are normal and have been stable for about six months. Longer prophylactic therapy may be needed, as in patients with tophi. Blood levels of urate are monitored periodically to ensure that the goal urate level is maintained.
What is New in Gout Therapy?
KRYSTEXXA
If you have more than one flare a year, it may be time to step up your gout treatment
Recurrent gout flares may be your body’s way of telling you that oral medicines aren’t doing enough to lower your uric acid level and prevent the harmful effects of out-of-control chronic gout.
Krystexxa has been helping gout patients for nearly 10 years. Studies show that one IV treatment every other week for about 6 months is all you may need to take control.
Oral gout medicines do not work the same way krystexxa does.
KRYSTEXXA has a different way of lowering uric acid levels, which is the key to stopping gout flares. In about 6 months, it can remove years of accumulated uric acid and Tophus your body
It helps to keep uric acid at very low levels thereby preventing acute attacks of gout, Tophus formation, prevent renal complications, hypertension and other damages related to elevated uric acid.
CCCHC offers Krystexxa treatments at 2 of our fully equipped infusion centers.
Ask your Doctor if you are a candidate for Krystexxa treatment and be referred to our center for further evaluation and treatment
Dietary changes — Changes in diet may reduce the frequency of gout attacks in some people. Because obesity is a risk factor for gout, as well as for many other health conditions (heart disease, diabetes, high blood pressure), losing weight is an important goal. However, starvation or fad diets are not recommended Diet guidelines for patients with gout have changed over time, and it is not completely clear which combination of foods is best.
The current recommendations include reducing intake of red meat and seafood, and increasing intake of low fat dairy products and complex carbohydrates.
Reducing intake of beer and hard alcohol (eg, gin, vodka) is recommended because these beverages have been shown to increase the risk of a gout attack.. A moderate intake of wine (one to two 5 ounce servings per day) is not likely to increase the risk of a gout attack.
High-fructose corn syrup products, (such as some types of non-diet soda) increase blood urate levels and are not recommended.
Coffee may decrease the risk of gout . Vitamin C (500 mg/day) has a mild urate-lowering effect and may be recommended.
Changes in diet are often recommended along with medications, but the reduction in blood urate levels due to diet change alone is modest (15 to 20 percent), even with very strict diets.
WHERE TO GET MORE INFORMATION — Your healthcare provider or your Rheumatologist (Doctors who specialize in Arthritis and gout) is the best source of information for questions and concerns related to your medical problem.
Because no two patients are exactly alike and recommendations can vary from one person to another, it is important to seek guidance from a provider who is familiar with your individual situation
For more information please contact CCCHC at 323-507-3734.